- Home
- From Doctor Burnout to Resilient Recovery
From Doctor Burnout to Resilient Recovery
Doctor burnout is more than just fatigue—it’s a state of emotional, physical, and mental exhaustion caused by prolonged stress, high demands, and insufficient recovery. It’s common among medical trainees, who often juggle long shifts, intense study schedules, and emotionally taxing clinical environments.
The World Health Organization defines burnout as a syndrome resulting from chronic workplace stress that has not been successfully managed. In the medical field, it manifests as:
- Emotional exhaustion
- Depersonalisation (feeling disconnected from patients or work)
- Reduced personal accomplishment
As Study Less and Still Blitz Your Medical Exams puts it:
“Burnout has reached epidemic levels among doctors with global prevalence rates ranging from 25–75%, and Australian levels ranging from 65–75%.”
Doctor burnout isn’t a personal failure—it’s a predictable outcome of an unsustainable system.
What is Doctor Burnout
Doctor burnout is the result of chronic, unmanaged stress. It’s not just feeling tired—it’s a state of emotional exhaustion, depersonalization, and reduced personal accomplishment.
Burnout is what happens when stress becomes constant, and recovery becomes absent.
Some early signs of burnout include:
- Feeling emotionally drained
- Losing empathy for patients
- Feeling ineffective or incompetent
- Constant fatigue, even after rest
- Cynicism and detachment
- Memory and concentration issues
- Physical symptoms (headaches, insomnia, weight changes)
The key differences between normal doctor stress and burnout
| Aspect | Normal Stress | Doctor Burnout |
|---|---|---|
| Duration | Short-term, situational | Long-term, chronic |
| Impact on Function | Enhances focus and performance | Impairs memory, decision-making, and empathy |
| Recovery | Possible with rest and coping strategies | Difficult without intervention or lifestyle change |
| Emotional State | Alert, motivated | Exhausted, cynical, detached |
| Physical Symptoms | Temporary tension or fatigue | Persistent fatigue, insomnia, illness |
| Mindset | “I can handle this” | “I can’t do this anymore” |
The Slow Burn of Doctor Burnout
Why It Builds—and Why It’s So Hard to Spot
Doctor burnout doesn’t happen overnight. It’s not a single bad shift or a tough exam—it’s the cumulative effect of chronic, unmanaged stress. It builds slowly, like water rising in a stress bucket. At first, you cope. You push through. You tell yourself it’s normal. But over time, the pressure becomes constant, and the recovery becomes absent. That’s when burnout takes hold.
For medical trainees, the causes are both systemic and personal—and they often interact in ways that make burnout feel inevitable.
 |
 |
Systemic Stressors:
|
Personal Stressors:
|
Systemic Stressors: The Environment You’re In
These are the structural pressures baked into the medical system:
- Long hours and shift work: Irregular rosters, night shifts, and overtime disrupt sleep, relationships, and recovery. Many junior doctors work 60+ hours a week, often with unpaid overtime.
- High-stakes exams: Fellowship exams are intense, competitive, and often repeated. The pressure to pass can dominate your life for months or years.
- Poor supervision or support: Many trainees report inadequate feedback, unclear expectations, and limited mentoring—especially during exam preparation.
- Bullying or toxic culture: Hierarchical environments can foster intimidation, exclusion, and emotional abuse. Nearly 40% of junior doctors report being bullied.
- Lack of control over schedules: Rigid rosters and unpredictable shifts make it hard to plan study, rest, or personal time.
- Emotional toll of patient care: Doctors deal with suffering, death, and complex ethical decisions daily. Without support, this emotional labor becomes draining.
- COVID-19 disruptions: The pandemic intensified stress, disrupted training schedules, and increased emotional fatigue. Many exams were postponed or restructured, adding uncertainty and pressure.
Personal Stressors: The Pressure You Put on Yourself
Even without systemic issues, many doctors carry internal expectations that amplify stress:
- Perfectionism: Many doctors are high achievers who fear failure and equate mistakes with incompetence.
- Imposter syndrome: Despite years of training, many feel like frauds—especially when comparing themselves to peers.
- Overstudying: The belief that more study equals better results leads to exhaustion and poor retention.
- Neglecting wellbeing: Exercise, sleep, and social connection are often sacrificed for study—ironically reducing performance and increasing burnout risk.
The "Push Through" Myth
Why Grit Alone Isn’t Enough—and What to Do Instead
In medicine, there’s a pervasive belief that the only way to succeed is to push through - keep going no matter how exhausted, overwhelmed, or emotionally drained you feel. This mindset is often passed down from senior doctors to trainees, reinforced by war stories of sleepless nights, endless study, and suffering as a rite of passage.
“You’ve been told that lots of study is what is going to get you through, so you probably have the mistaken belief that more is better.”
But here’s the truth: pushing through isn’t resilience—it’s denial.
The “push through” mentality teaches doctors to ignore their own needs. It glorifies overwork and treats rest, recovery, and wellbeing as weaknesses or luxuries. Over time, this leads to:
- Chronic fatigue
- Poor memory and concentration
- Emotional detachment
- Increased medical errors
- Burnout and depression
Instead of draining the stress bucket, this mindset fills it faster. You keep going until the bucket overflows - and by then, it’s often too late.
So where does the "push through" belief come from?
This myth is rooted in outdated cultural norms:
- “I suffered, so you should too.” Senior doctors often pass down the belief that suffering builds character.
- “Real doctors don’t complain.” Expressing vulnerability is seen as weakness.
- “You just need to work harder.” Struggling is interpreted as laziness or incompetence.
- “Rest is for after the exam.” Recovery is postponed indefinitely.
These beliefs are not only false—they’re dangerous.
The “push through” mentality may be common in medicine, but modern performance science tells a very different story.
What Modern Performance Science Tells Us
Why Recovery, Sleep, Exercise, and Mindfulness Are Non-Negotiable for Doctors
The “push through” mentality may be common in medicine, but modern performance science tells a very different story. Whether you're an elite athlete or a medical trainee, peak performance requires deliberate recovery. Ignoring this science doesn’t make you stronger—it makes you slower, foggier, and more vulnerable thinking errors and to burnout.
Let’s break down the key pillars:
 |
 |
 |
 |
1. Recovery Improves Performance |
2. Sleep Consolidates Memory |
3. Exercise Boosts Cognition |
4. Mindfulness Reduces Stress |
1. Recovery Improves Performance
Elite athletes don’t just train hard—they recover hard. Recovery is where adaptation happens. Without it, performance declines, injuries increase, and burnout sets in.
In elite sports, sports psychology is now a core part of training, helping athletes manage stress, recover mentally, and sustain long-term performance. This same model is increasingly relevant for doctors, who face similar high-stakes environments.
“Sports psychiatrists are uniquely trained to bridge the gap between mental illness and mental performance, providing diagnostic and therapeutic expertise while also helping athletes build cognitive strategies for resilience and peak functioning.”
Doctors, like athletes, need structured recovery to maintain cognitive sharpness, emotional regulation, and resilience.
2. Sleep Consolidates Memory
Sleep isn’t just rest—it’s active memory processing. During sleep, especially deep and REM stages, the brain consolidates short-term memories into long-term storage. This is essential for learning, recall, and exam performance.
Research shows that sleep deprivation impairs memory, attention, and decision-making, with effects comparable to alcohol intoxication.
“Sleep memory consolidation involves strengthening neural connections that form memories… Doctors are more likely to recall their studies later if they have had a good night’s sleep.”
Late-night cramming may feel productive—but it’s counterproductive for retention and recall.
3. Exercise Boost Cognition
Exercise isn’t just good for your body—it’s a powerful cognitive enhancer. Physical activity increases blood flow to the brain, stimulates neurogenesis, and improves mood, focus, and memory.
Harvard psychiatrist Dr. John Ratey describes exercise as “Miracle-Gro for the brain,” showing that it improves learning on three levels: neurotransmitter balance, neurogenesis, and synaptic plasticity
“Exercise primes your brain to learn and allows your brain to retain information easier”
Even short bursts of moderate to high-intensity exercise before study sessions have been shown to improve encoding and retrieval.
4. Mindfulness and Breathwork Reduce Stress
Mindfulness and breathwork activate the parasympathetic nervous system—your body’s “rest and digest” mode. This reduces cortisol, lowers heart rate, and improves emotional regulation.
A systematic review found that slow, deep breathing improves heart rate variability, reduces anxiety, and enhances cognitive performance.
“Deep breathing promotes changes in the autonomic nervous system… and increases alpha wave activity, a sign of good cognitive performance.”
Techniques like 4-7-8 breathing or diaphragmatic breathwork are simple, portable, and effective—even during shifts or study breaks.
Putting Performance Science Into Your Study
The “push through” mindset tells you to ignore your body, your emotions, and your limits. But modern performance science—and real-world experience—shows that working smarter, not harder, is the key to long-term success.
Here’s what you can do instead:
1. Schedule Recovery Like You Schedule Study
Just like athletes plan rest days, you need to build recovery into your routine. This includes:
- Short breaks during study (e.g. 50/10 rule: 50 minutes study, 10 minutes break)
- Daily decompression (walks, music, hobbies, social time)
- Weekly recovery (a full day off from study/work if possible)
- Pre-exam tapering (reduce study load 1–2 weeks before the exam to stay fresh)
Think of recovery as a performance enhancer—not a reward.
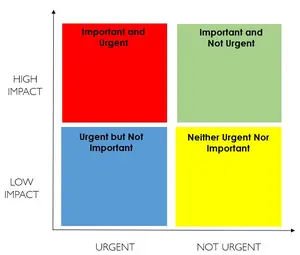
2. Use the Stress Bucket Model
Visualise your stress like water in a bucket. Instead of letting it overflow:
- Identify what’s filling it (e.g. shift work, study pressure, toxic environments)
- Find your taps (e.g. exercise, sleep, breathwork, social connection)
- Avoid false taps (e.g. alcohol, doomscrolling, overstudying)
Track your stress daily and adjust your habits accordingly.
3. Switch from Passive to Active Recovery
Not all rest is equal. Scrolling on your phone might feel like a break—but it doesn’t restore your energy. Instead, try:
- Mindful breathing (4-4 or 4-7-8 technique)
- Nature walks
- Creative outlets (music, journaling, art)
- Laughter and connection (talk to someone who gets it)
These activities activate your parasympathetic nervous system, helping your body and brain reset.
4. Train Like a Cognitive Athlete
Use the same principles elite performers use:
- Sleep: Prioritise 7–9 hours. It’s when your brain consolidates memory.
- Exercise: Even 10–20 minutes of movement boosts focus and mood.
- Nutrition: Fuel your brain with whole foods, not just caffeine and sugar.
- Hydration: Dehydration impairs concentration and memory.
5. Use Micro-Resets During the Day
Between patients, study blocks, or meetings, take 30–60 seconds to:
- Stand up and stretch
- Take 3–5 deep breaths
- Close your eyes and visualize a calm place
- Repeat a grounding phrase (e.g. “I’ve got this. One step at a time.”)
These micro-resets prevent stress from accumulating.
6. Create a Personal Resilience Plan
Build a toolkit that works for you. Include:
- Your top 3 stressors
- Your most effective taps
- A weekly recovery ritual
- A go-to breathing technique
- A support person you can call
Keep it visible—on your desk, phone, or fridge.
7. Redefine Success
Success isn’t just about passing exams. It’s about:
- Staying well enough to keep going
- Learning how to recover and adapt
- Building habits that will serve you for life
- Becoming the kind of doctor who thrives—not just survives
Final Thoughts
Burnout Isn’t a Personal Failure—It’s a Systemic Signal
Burnout isn’t a sign that you’re not strong enough. It’s not a reflection of your intelligence, your dedication, or your worth as a doctor. It’s a predictable outcome of a system that demands too much, gives too little, and rarely teaches you how to care for yourself while caring for others.
But here’s the truth: burnout is not inevitable.
Yes, the system is flawed. Yes, the workload is intense. Yes, the expectations—both internal and external—can feel crushing. But within that reality, there is still space for change. There is still room for awareness, support, and resilience strategies that can interrupt the cycle and help you recover.
Awareness Is the First Step
Burnout often creeps in unnoticed. You don’t wake up one day and feel “burnt out.” It builds slowly—through skipped meals, sleepless nights, missed birthdays, and the quiet erosion of joy. Recognising the early signs—emotional exhaustion, cynicism, disconnection—is the first act of self-care.
Support is Essential
You don’t have to do this alone. Whether it’s a mentor, a coach, a colleague, a psychologist, or a friend—connection is protective. Talking about your experience doesn’t make you weak. It makes you human. And it opens the door to healing.
Resilience is Learnable
Resilience isn’t about pushing through. It’s about bouncing back. It’s about learning how to rest, how to reflect, how to reset. It’s about building habits that protect your energy, sharpen your focus, and sustain your passion for medicine.
You can:
- Use the stress bucket model to manage your load
- Build recovery into your study and work routines
- Challenge thinking traps and perfectionism
- Practice mindfulness and breathwork
- Redefine success beyond exams and titles
- Consider this four burner theory on balancing work, health, family and friends.
Burnout is not the end of the road. It’s a turning point. With the right tools, mindset, and support, you can recover—not just to survive, but to thrive. You can reconnect with your purpose, your patients, and yourself.
And when you do, you’ll not only be a better doctor—you’ll be a healthier, more fulfilled human being.