- Home
- From Doctor Burnout to Resilient Recovery
- Signs of Burnout
Self-Awareness: Recognizing Early Signs of Burnout
In medicine and other high-pressure professions, burnout is often misunderstood. It’s not a sign of strength or commitment—it’s a warning sign. A signal that something needs to change. Yet, in many medical cultures, burnout is worn like a badge of honor, a rite of passage that proves you’re working hard enough. Recognising the early signs of burnout is essential to prevent long-term damage.
A study published by the Medical Journal of Australia in 2009 reported a 69% incidence of burnout among junior doctors, but interns were excluded from this study
Burnout doesn’t arrive with fanfare. It creeps in silently, often disguised as dedication, resilience, or the pursuit of excellence. Junior doctors, in particular, are vulnerable. They’re navigating demanding rosters, emotionally intense environments, and the pressure of looming exams—all while trying to maintain a semblance of personal life.
What is Burnout
Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged and unmanaged stress. It’s not just feeling tired—it’s feeling depleted, disconnected, and defeated.
The World Health Organization defines burnout as an occupational phenomenon, not a medical condition, but its consequences are serious. Burnout manifests in three key ways:
Emotional Exhaustion
 |
Depersonalization
 |
Reduced Personal Accomplishment |
|
Feeling drained, overwhelmed, and unable to cope. |
Becoming cynical, detached, or indifferent toward work and patients. |
Feeling ineffective, unproductive, or like you’re failing. |
And the consequences are far-reaching:
“Burnout leads to increased medical errors, reduced work hours, and increased suicidal ideation; therefore, we all have a vested interest in preventing burnout”
Why Self-Awareness is Crucial
In the demanding world of medicine, self-awareness isn’t just a soft skill—it’s a survival tool. For junior doctors, who often operate under extreme pressure, long hours, and high expectations, recognizing the early signs of burnout can be the difference between thriving and crashing.
Increasing self-awareness increases resilience and your ability to respond well to stress.
Self-awareness allows doctors to tune into their physical, emotional, and cognitive states. It’s about noticing when something feels off—when fatigue becomes chronic, when motivation dips, or when anxiety starts to cloud judgment. These are often the early signs of burnout, and catching them early is key to preventing long-term damage.
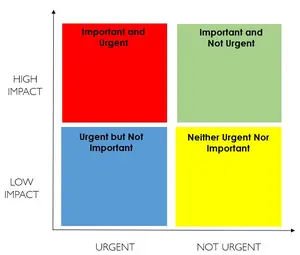
The Power of the Pause
In high-pressure environments like medicine, where decisions are rapid and stakes are high, the ability to pause—even briefly—can be transformative. The pause is not a delay. It’s a moment of clarity, a reset, and a gateway to self-awareness.
As we say in our book, increasing self-awareness gives doctors the ability to
“pause and consider before acting”
This pause is where choice lives. It’s where you shift from reacting to responding.
Why the Pause Matters
Burnout often builds silently. Doctors push through fatigue, ignore irritability, and suppress anxiety. But these are the early signs of burnout, and without awareness, they escalate. The pause helps you notice these signs before they become chronic.
“Between stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom.” — Viktor Frankl
This space—the pause—is where you can:
- Recognise your emotional state
- Interrupt negative thought patterns
- Choose a healthier response
- Prevent automatic reactions driven by stress
Early Signs of Burnout for Junior Doctors
Burnout doesn’t happen overnight. It’s a slow, cumulative process that often goes unnoticed until it begins to affect performance, wellbeing, and relationships. For doctors, especially junior doctors navigating exams, shift work, and emotionally demanding environments, recognizing the early signs of burnout is essential for intervention and recovery.
Here are some of the most common early indicators:
 |
1. Chronic FatigueThis isn’t just feeling tired after a long shift—it’s a persistent exhaustion that doesn’t improve with rest. It’s physical, emotional, and cognitive depletion. Doctors may feel like they’re running on empty, struggling to find energy for even basic tasks. Over time, this fatigue erodes motivation and resilience, making it harder to engage with study, work, or relationships. |
 |
2. Sleep DisturbancesSleep is often one of the first casualties of burnout. Difficulty falling asleep, frequent waking, or waking too early are common patterns. Poor sleep not only worsens fatigue but also impairs memory, concentration, and emotional regulation—creating a vicious cycle that accelerates burnout. Over time, this sleep disruption can also diminish your ability to cope with stress, making even routine tasks feel overwhelming. |
 |
3. Loss of Motivation and Increased CynicismTasks that once felt purposeful begin to feel meaningless. Doctors may start to question their career choice, feel disconnected from their patients, or dread upcoming exams. Cynicism can manifest as sarcasm, irritability, or emotional detachment. This erosion of meaning and motivation is a hallmark of emotional exhaustion. |
 |
4. Memory and Concentration IssuesBurnout affects cognitive function. Doctors may find it harder to retain information, focus during study, or recall facts under pressure. This can be especially distressing during exam preparation, where memory lapses feel like personal failure. But as the book explains, these issues are often a result of stress and fatigue—not lack of ability. |
 |
5. Social WithdrawalIsolation is both a symptom and a risk factor for burnout. As energy and motivation decline, doctors may withdraw from social activities, even those they once enjoyed. This loss of connection can deepen feelings of loneliness and reduce access to emotional support—further compounding stress. Over time, this disconnection can also erode a doctor’s sense of identity and belonging, making it harder to re-engage even when the opportunity arises. |
Why These Signs Matter and What Can You Do
Each of these symptoms may seem minor on its own. But together, they form a pattern—a warning system. Recognizing these early signs of burnout allows doctors to take proactive steps: adjusting workloads, seeking support, improving sleep hygiene, or engaging in restorative activities.
As we emphasize throughout our book, burnout is not a personal failure—it’s a systemic issue that requires awareness, compassion, and strategic intervention.
1. Set Boundaries
Why it matters: Junior doctors often feel pressure to be constantly available, but this leads to chronic fatigue and emotional exhaustion.
How to apply it:
- Schedule protected time for study, rest, and personal activities—treat it like a clinical appointment.
- Limit overtime: Say no to extra shifts during exam periods unless absolutely necessary.
- Use roster requests: Advocate for study-friendly rosters or lighter rotations before exams
2. Seek Support
Why it matters: Isolation and stigma around mental health are common barriers for junior doctors.
How to apply it:
- Mentorship: Connect with a senior doctor who understands the pressures of exams and clinical work.
- Peer networks: Join junior doctor forums or WhatsApp groups for shared study tips and emotional support.
- Professional help: Access hospital wellbeing programs or confidential counselling services—many are free or subsidized.
3. Adjust Workload (If Possible)
Why it matters: High patient loads and unpredictable rosters are major contributors to burnout
How to apply it:
- Locum shifts: Consider casual or part-time work during exam-heavy months.
- Roster flexibility: Request fewer night shifts or on-calls around key study periods.
- Use leave strategically: Take annual or study leave before exams to reduce pressure.
4. Stay Connected
Why it matters: Social isolation worsens stress and reduces resilience
How to apply it:
- Plan short social breaks: Even a 30-minute coffee with a friend can help reset your mood.
- Keep hobbies alive: Whether it's music, sport, or gaming—make time for what brings you joy.
- Join interest groups: Many hospitals have junior doctor clubs or wellness committees.
5. Practice Self-Compassion
Why it matters: Many junior doctors are high achievers who struggle with self-criticism.
How to apply it:
- Reframe setbacks: Missing a study goal or making a clinical error doesn’t define your worth.
- Use affirmations: Remind yourself, “I’m doing my best in a tough environment.”
- Celebrate small wins: Completing a topic, surviving a tough shift—these are victories.
6. Mindfulness & Recovery
Why it matters: Mindfulness helps manage anxiety and improves focus during study and work.
How to apply it:
- Try short meditations: Use apps like Smiling Mind (Australian-based) or Headspace.
- Practice breathing techniques: Box breathing or 4-7-8 breathing during breaks.
- Move your body: Even light stretching or a walk between shifts can reduce stress.
Final Thought on Early Signs of Burnout
Burnout is not a personal weakness—it's a natural response to sustained stress in a demanding environment. For junior doctors, the pressure of clinical responsibilities, exam preparation, and personal expectations can create a perfect storm. Recognizing the early signs and taking proactive steps is not just about surviving—it’s about preserving your passion for medicine and your overall wellbeing.
You are not alone in this journey. Many have walked this path and found ways to thrive by setting boundaries, seeking support, and prioritizing recovery. Small, consistent changes can make a big difference. Whether it's carving out time for a walk, saying no to an extra shift, or reaching out to a mentor, each step is a move toward balance.
Remember: your health matters just as much as your patients’. Taking care of yourself is not selfish—it’s essential.