- Home
- From Doctor Burnout to Resilient Recovery
- Doctors and Stress
Doctors and Stress: Understanding the Stress Bucket Model
Doctors and stress are inseparable—especially in high-pressure environments like hospitals, clinics, and exam preparation. While some stress is expected and even necessary to stay alert and perform under pressure, unmanaged stress can quietly accumulate until it leads to burnout, anxiety, and emotional exhaustion.
That’s where the Stress Bucket Model comes in. It’s a simple yet powerful metaphor that helps doctors visualize how stress builds up—and how it can be drained before it overflows.
Visualizing Stress Like a Bucket
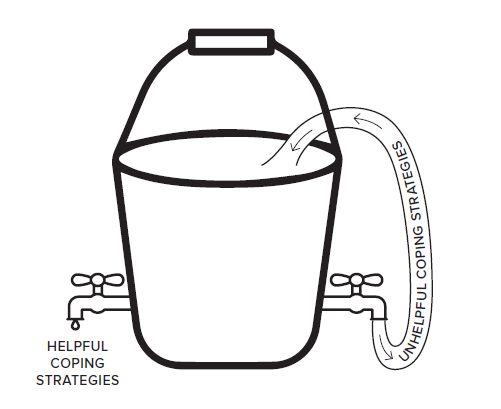
Imagine your mind as a bucket. Every stressor—clinical workload, exam pressure, poor sleep, difficult patients, toxic environments—adds water to the bucket. For doctors, stress pours in from multiple sources, often simultaneously and without warning.
If the water level rises too high, the bucket overflows. That overflow is burnout, emotional collapse, or a breakdown in performance.
But here’s the key insight: your bucket has taps. These taps represent your coping strategies—the healthy habits and tools that help you drain stress before it overwhelms you.
Six Things that Fill the Stress Bucket for Doctors
Doctors face a unique combination of chronic stressors, many of which are systemic and unavoidable. These include:
1. Clinical Demands |
2. Academic Pressure |
 |
|
 |
|
3. Emotional Load |
4. Workplace Culture |
 |
|
 |
|
5. Personal Life Stressors |
6. Systemic and Structural Stress |
 |
|
 |
|
These stressors accumulate silently. Without intervention, they fill the bucket faster than it can drain.
4 Things that Drain the Stress Bucket for Doctors
Healthy coping strategies—your taps—help release stress and prevent overflow. These taps are deliberate, restorative actions that support physical, emotional, and cognitive recovery and reduce the chances of burnout.
1. Physical Taps |
2. Emotional Taps |
 |
|
 |
|
3. Cognitive Taps |
4. Social Taps |
 |
|
 |
|
These taps don’t just relieve stress—they build resilience. The more consistently you use them, the more capacity your bucket has to handle future stress.
⚠️ Watch Out for False Taps
Not all coping strategies are helpful. Some feel like relief in the moment but actually add more water to the bucket. These are called false taps.
- Excessive alcohol or substance use: Numbs stress temporarily but disrupts sleep, mood, and cognition.
- Overstudying: Feels productive but leads to fatigue and poor retention.
- Procrastination or avoidance: Delays stress but increases anxiety later.
- Doomscrolling or passive screen time: Distracts but doesn’t restore.
- Venting without reflection: Can reinforce negativity without resolution.
- Skipping meals or sleep to “get ahead”: Sacrifices recovery for short-term gain.
False taps are deceptive. They offer short-term relief but create long-term damage. Recognizing them is the first step to replacing them with healthier alternatives.
Why It Matters for Doctors
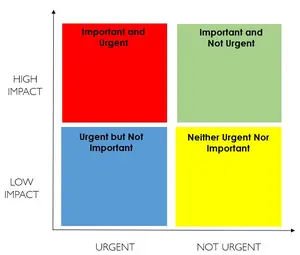
Doctors often operate in environments where stress is constant and recovery is rare. The Stress Bucket Model helps shift the mindset from “just push through” to “manage and recover.” It encourages proactive self-awareness and gives doctors a framework to:
- Identify what’s filling their bucket
- Recognize when it’s close to overflowing
- Use deliberate strategies to drain it
- Avoid false taps that worsen stress over time
This model is especially useful for medical trainees, who are often juggling clinical duties, study schedules, and personal responsibilities—all while navigating a system that rarely prioritizes their wellbeing.
How to Use the Model
Doctors can use the Stress Bucket Model to:
- Track daily stressors and coping strategies.
- Consider any thinking traps you could be falling into.
- Identify which taps are working—and which aren’t
- Replace false taps with healthy ones
- Build resilience through deliberate recovery
- Prevent burnout by managing stress proactively
Final Thought on Doctors and Stress
Doctors and Stress Are Inseparable—But Burnout Doesn’t Have to Be
Stress is part of the job. Whether you're a junior doctor preparing for exams, a registrar managing a full patient load, or a consultant leading a team, stress is woven into the fabric of medical life. But while doctors and stress may be inseparable, burnout is not inevitable.
The key difference lies in how you manage that stress—and how early you intervene.
The Stress Bucket Model offers a simple but powerful way to visualize your stress load. It helps you understand that stress isn’t just something to endure—it’s something you can track, manage, and release. By identifying what’s filling your bucket and what’s draining it, you gain clarity. You begin to see patterns. And most importantly, you start to take back control.
This model doesn’t ask you to be perfect. It doesn’t expect you to eliminate stress entirely. Instead, it encourages awareness over avoidance, and strategy over struggle.
It’s About Building Habits That Protect You
- It’s about recognizing when your bucket is getting full—and knowing how to release the pressure.
- It’s about replacing false taps with real ones that restore your energy.
- It’s about making space for recovery, even in a system that rarely gives you permission to pause.
- It’s about choosing sustainability over sacrifice with sustainable work life practices.
Awareness Is the First Act of Self-Compassion
When you understand your stress, you can manage it. When you manage it, you protect your wellbeing. And when you protect your wellbeing, you not only survive in medicine—you thrive.
So no, you don’t need to be perfect.
You just need to be aware.
And that awareness is your first step toward resilience.