- Home
- From Doctor Burnout to Resilient Recovery
- Sleep Hygiene
Sleep Hygiene and Memory Consolidation: Refuel Your Cognitive Engine
Sleep is your fuel stop. Just like a Formula 1 car can’t finish a race without pulling into the pit lane, your brain can’t perform at its best without rest—and sleep hygiene is the maintenance protocol that keeps your cognitive engine running smoothly. Skip the pit stop, and even the most finely tuned machine will overheat, misfire, or crash out of the race.
When sleep hygiene is neglected—irregular sleep schedules, late-night screen time, heavy meals before bed - your cognitive engine begins to sputter. Your memory falters. Your emotional regulation weakens. Your ability to retain and retrieve study material plummets. You might still be moving - but you’re no longer racing at peak performance.
In our book Study Less and Still Blitz Your Medical Exams, we make it clear: sleep is not a luxury—it’s a non-negotiable performance enhancer. It’s the difference between cruising through your exams with clarity and confidence, or stalling out under pressure.
If you’re a junior doctor juggling long shifts, high-stakes exams, and personal responsibilities, sleep might feel like the first thing to sacrifice. But science - and experience - say otherwise. In fact, sacrificing sleep is like skipping a tire change mid-race: it might save time in the short term, but it’s a guaranteed blowout waiting to happen.
Here we explore:
- why sleep hygiene is critical for memory consolidation,
- how poor sleep sabotages your performance, and
- what you can do to reclaim your rest, your resilience, and your competitive edge.
Because in the high-speed world of medicine, your brain is your vehicle—and sleep hygiene is the pit stop that keeps you in the race.
Sleep Science: Why it Matters for Learning and Memory
Sleep isn’t just rest—it’s active brainwork, and sleep hygiene is the protocol that ensures this brainwork happens effectively. When your sleep hygiene is poor—irregular schedules, late-night screen time, heavy meals before bed—you’re not just tired. You’re compromising your brain’s ability to learn, remember, and perform.
During sleep, your brain processes, organizes, and stores the information you’ve absorbed throughout the day. This process is called memory consolidation, and it’s essential for learning—especially for junior doctors who are constantly absorbing new clinical knowledge, procedures, and protocols.
Sleep occurs in cycles, alternating between non-REM (NREM) and REM stages. Each stage plays a unique role in memory formation:
- Slow-wave sleep (SWS), a deep NREM stage, is crucial for consolidating declarative memory - facts, concepts, and textbook knowledge.
- REM sleep, associated with dreaming, helps consolidate procedural memory - skills, routines, and emotional learning.
During these stages, your brain replays and strengthens neural connections, transferring memories from short-term storage in the hippocampus to long-term storage in the neocortex. This transfer is what allows you to recall what you studied days or weeks later—not just hours after reading it.
“Sleep compared to wakefulness preferentially benefits certain memories,”
But here’s the catch: without adequate sleep hygiene, this process is disrupted. You may read the same page five times and still forget it the next day—not because you didn’t study hard enough, but because your brain didn’t have time to file it away.
In our book 'Study Less and Still Blitz Your Medical Exams', we emphasize that sleep is not a passive state—it’s a non-negotiable performance enhancer. That sleep hygiene is just as important as study technique. Without it, your brain can’t do the behind-the-scenes work that turns information into knowledge.
Poor sleep hygiene—like studying late into the night, using screens before bed, or skipping wind-down routines—can sabotage your ability to retain and retrieve information. It’s like trying to race with a misfiring engine: you might still be moving, but you’re not performing at your best.
By prioritizing sleep hygiene, you give your brain the conditions it needs to consolidate memory, regulate emotions, and prepare for the next day’s challenges. It’s not just about getting more sleep—it’s about getting better sleep.
Sleep Deprivation: Like Driving Drunk in Your Own Brain
Sleep deprivation doesn’t just make you tired—it impairs your brain in ways that mimic intoxication.
Studies show that being awake for 18–24 hours can impair cognitive performance as much as a blood alcohol level of 0.05–0.10.
That’s above the legal limit for driving in Australia.
Sleep-deprived brains struggle with:
- Attention and focus
- Decision-making
- Emotional regulation
- Working memory
- Reaction time
For junior doctors, this is especially dangerous. You’re expected to make fast, accurate decisions, absorb complex material, and perform under pressure. Without sleep, your ability to do any of that drops sharply.
Sleep Hygiene for Junior Doctors - 6 Things You Can Do Now
Staying with the metaphor of racing, your sleep routine like a Formula 1 pit crew prepping a race car. Every detail matters. From tyre pressure to fuel levels, nothing is left to chance—and the same should apply to your sleep hygiene. As a junior doctor, your brain is your vehicle, and sleep is the maintenance that keeps it race-ready.
Here’s are 6 things you can do today to fine-tune your sleep hygiene so your cognitive engine runs at peak performance:
1. Study Earlier in the Day |
2. Wind Down with Quiet Time |
3. Avoid Screens Before Bed |
 |
 |
 |
4. Eat Light and Early |
5. Create a Sleep-Friendly Environment |
6. Stick to a Consistent Schedule |
 |
 |
 |
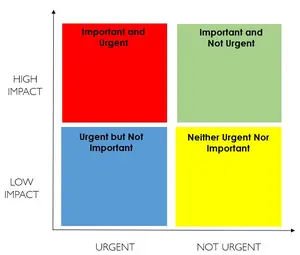
1. Study Earlier in the Day
We emphasize that junior doctors often fall into the trap of cramming late at night, believing more hours equals better results. However, this approach leads to exhaustion, poor retention, and burnout. The authors advocate for morning study sessions, aligning with the brain’s natural alertness cycle and leveraging the circadian rhythm for optimal cognitive performance.
Scientific Backing: Morning study enhances encoding and consolidation of memory. Sleep-deprived learning, especially late-night cramming, impairs hippocampal function, reducing long-term retention.
Practical Tip: Use your morning energy for deep learning and problem-solving. Reserve evenings for light review, reflection, or planning.
2. Wind Down with Quiet Time
We compare this to a Formula 1 pit stop—essential for recovery. Quiet time before bed helps reduce cortisol and prepares the brain for memory consolidation during sleep.
Recommended Activities:
- Gentle stretching or yoga
- Reading a physical book
- Journaling
- Guided meditation or calming music
Why It Matters: This transition helps shift from sympathetic (fight-or-flight) to parasympathetic (rest-and-digest) mode, essential for restorative sleep.
Practical Tip: Create a wind-down ritual that’s screen-free and emotionally neutral. Even 30 minutes can make a difference.
3. Avoid Screens Before Bed
Screen time before bed can be a major disruptor of sleep hygiene. Blue light suppresses melatonin, delaying sleep onset and reducing REM sleep—critical for emotional regulation and procedural memory.
Alternatives:
- Use paper notes for evening review
- If screens are necessary, use blue-light filters or night mode
Scientific Backing: Studies show that screen exposure within 1 hour of bedtime can reduce melatonin by up to 50%, impairing sleep quality.
Practical Tip: Power down devices at least 60 minutes before bed. If unavoidable, wear blue-light blocking glasses.
4. Eat Light and Early
Heavy meals late in the evening can cause acid reflux, blood sugar spikes, and digestive discomfort, all of which impair sleep. Finishing dinner 2–3 hours before bed and choosing sleep-friendly snacks if needed can help here.
Sleep-Friendly Snacks:
- Banana (rich in magnesium and tryptophan)
- Yogurt (contains calcium, which helps process melatonin)
- Almonds (source of magnesium and melatonin)
Avoid:
- Caffeine after 2 p.m.
- Alcohol close to bedtime (reduces REM and fragments sleep)
Practical Tip: Track how your evening meals affect your sleep and adjust accordingly.
5. Create a Sleep-Friendly Environment
Our book stresses the importance of environmental cues in reinforcing sleep habits. Your bedroom should be a sanctuary—not a study zone.
Optimize Your Space:
- Keep the room cool (18–20°C)
- Use blackout curtains
- Minimize noise (white noise machines or earplugs)
- Remove clutter and digital distractions
Why It Matters: Environmental consistency helps condition your brain to associate your bed with sleep, not stress or stimulation.
Practical Tip: Avoid studying or scrolling in bed. This weakens the bed-sleep association and can lead to insomnia.
6. Stick to a Consistent Schedule
Shift work and irregular rosters are common for junior doctors. We acknowledge this challenge but emphasize the importance of protecting sleep windows and planning recovery time.
Why It Matters: Irregular sleep patterns confuse your circadian rhythm, leading to poor sleep quality and daytime fatigue.
Scientific Backing: Even small shifts in bedtime (e.g., 1–2 hours) can disrupt melatonin production and sleep architecture.
Practical Tip: Go to bed and wake up at the same time daily—even on weekends. If your schedule changes, adjust gradually.
Sleep Hygiene for Shift Workers
Junior doctors often work rotating shifts, which wreak havoc on sleep patterns. But you can still protect your sleep:
- Prioritize sleep: Treat it like a critical appointment.
- Use naps strategically: Short naps (10–30 minutes) boost alertness; longer naps (60–90 minutes) aid memory consolidation.
- Manage light exposure: Use bright light during night shifts and block light during daytime sleep.
- Avoid caffeine late in your shift: It can linger in your system for hours.
- Plan your transition to days off: Gradually shift your sleep schedule to avoid jet lag-like symptoms
The Sleep Health Foundation recommends:
“Shift workers should aim for 7–9 hours of sleep and consider napping strategies to sustain alertness,”
Final Thoughts
If you’ve ever asked, “Is being a doctor stressful because it robs you of rest?”—the answer is yes. But it doesn’t have to.
Sleep is not a weakness. It’s not a luxury. It’s a strategic tool for memory, focus, emotional resilience, and long-term wellbeing.
As a junior doctor, your brain is your most valuable asset. Protect it. Fuel it. Let it rest.
Because when you sleep better, you study smarter, work safer, and live stronger.